New Jersey Peripheral Arterial Disease Treatment
Understanding Peripheral Arterial Disease (PAD)
Peripheral arterial disease (PAD) affects around 20 percent of Americans age 50 and older. As cholesterol and scar tissue accumulates over the years, plaque builds up and begins to clog the arteries. The clogged arteries cause decreased blood flow to the legs, which can result in pain when walking, and eventually gangrene and amputation.
When faced with the symptoms of PAD many people simply assume the pain is part of the aging process and accept it as their new normal. However, there are many options available to you to combat the discomfort and better your overall health. If you are experiencing chronic pain in your legs, we urge you to contact our clinical team at The Vascular Institute at AMI to learn how peripheral arterial disease treatment can help improve your daily quality of life.
Call (877) 595-9512 or contact us online to learn more about peripheral arterial disease treatment in New Jersey.
Identifying Symptoms of Peripheral Arterial Disease
The most detectable symptom of PAD is cramping that typically occurs in the legs or hips and is often experienced when engaged in a physical activity such as exercising, or even simply walking. Additionally, you may feel numbness, tingling, or weakness in your legs or feet.
Other symptoms include:
- Cold legs/feet
- Burning or aching pain in feet/toes
- Sore or wound on leg/foot that won’t heal
- Color change in skin on legs/feet
- Loss of hair on legs
- Night pains in legs/feet that inhibits sleep
Many people simply live with their pain, assuming it is a normal part of aging, rather than reporting it to their doctor.
Understanding the Risk Factors for PAD
Those who are at highest risk for Peripheral Arterial Disease are:
- Over age 50
- Smokers
- Diabetic
- Overweight
- Inactive (and do not exercise)
- Have high blood pressure or high cholesterol or high lipid blood test
- Have a family history of vascular disease, such as PAD, aneurysm, heart attack or stroke

TREATMENT OPTIONS
PAD treatment usually includes several approaches, including weight loss, eating habit changes, medication, and revascularization. The process of revascularization involves restoring the blood flow in the affected artery.
If you have tired, achy, and painful legs, it could be peripheral arterial disease. The Vascular Institute at AMI offers effective procedures to restore your blood flow. Our team specializes in minimally invasive revascularization procedures at the state-of-the-art facility.
Reach out to us at (877) 595-9512 today with any questions you may have. We look forward to hearing from you!
Vascular Disease Testing and Screening
The Vascular Institute offers free ABI screenings. We invite you to schedule your ABI test so that we can start your peripheral vascular disease treatment.
If you do not currently have symptoms that does not mean you are not at risk for vascular disease. If you have risk factors such as:
- Age 65 or older
- Age 50 or older with high cholesterol, diabetes, or smoking history
- Strong family history of heart or vascular disease or aortic aneurysm
If you have symptoms, you should consider getting an ABI test to see if they are related to peripheral vascular disease.
Symptoms include:
- Pain in the thigh, calf or buttocks with walking certain distances
- Non-healing wounds on your feet or lower extremities
- Pain in the leg or foot while resting relieved by hanging over the bed
Ankle Brachial Index
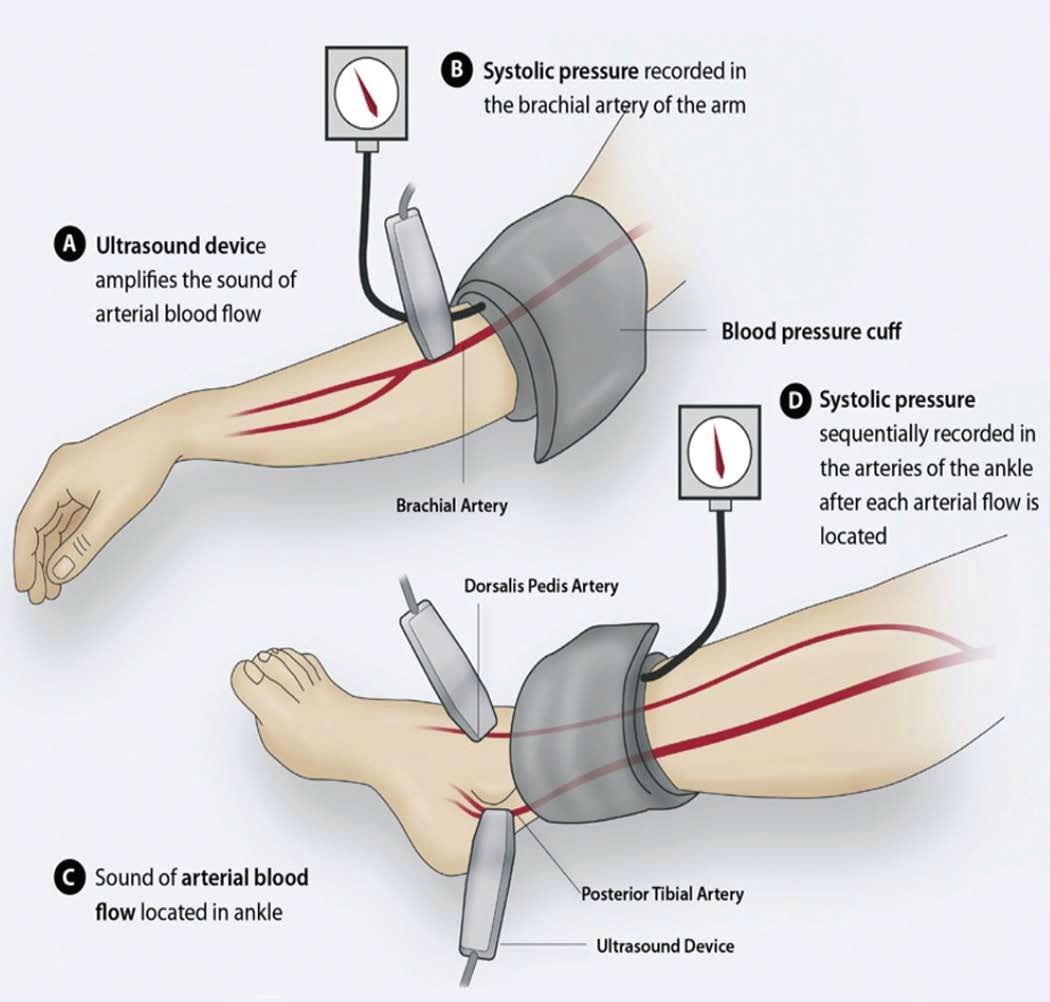
The ABI is a simple, painless test that compares the blood pressure reading in the arm and ankle. It is a direct measure of fatty plaque buildup in leg arteries and an indirect gauge of plaque accumulations throughout the entire cardiovascular system. This method is entirely non-invasive and completely painless.
To schedule your ABI Screening, please click here.
Treatments
Lifestyle Changes
Often PAD can be treated with lifestyle changes. Smoking cessation and a structured exercise program are often all that is needed to alleviate symptoms and prevent further progression of the disease.
Medication
Medications that lower cholesterol or control high blood pressure may be prescribed. Medication also is available that been shown to significantly increase pain-free walking distance and total walking distance in individuals with intermittent claudication. Other medications that prevent blood clots or the buildup of plaque in the arteries are available as well.
Exercise
Research has shown that supervised regimented exercise programs can improve symptoms of claudication. This should be attempted for at least three months for any occupational or vocational life limiting claudication prior to considering invasive therapies.
Angioplasty and stenting
Interventional radiologists pioneered angioplasty and stenting, which was first performed to treat peripheral arterial disease. Using imaging for guidance, the interventional radiologist threads a catheter through the femoral artery in the groin, to the blocked artery in the legs. Then the interventional radiologist inflates a balloon to open the blood vessel where it is narrowed or blocked. In some cases, this is then held open with a stent, a tiny metal cylinder. This is a minimally invasive treatment that does not require surgery, just a nick in the skin the size of a pencil tip.
Balloon angioplasty and stenting have generally replaced invasive surgery as the first-line treatment for PAD. Early randomized trials have shown interventional therapy to be as effective as surgery for many arterial occlusions, and in the past years, a very large clinical experience in centers throughout the world has shown that stenting and angioplasty are preferred as a first-line treatment for more and more processes throughout the body.
Atherectomy
With this treatment, a tiny catheter is inserted into the artery at the site of blockage that is able to “shave” or “cut” the plaque from the inside of the artery and remove it from the patient.
Testing
Ankle Brachial Index
The ABI is a simple, painless test that compares the blood pressure reading in the arm and ankle. It is a direct measure of fatty plaque buildup in leg arteries and an indirect gauge of plaque accumulations throughout the entire cardiovascular system. This method is entirely non-invasive and completely painless.
The blood pressure in your arms and ankles is checked using a regular blood pressure cuff and a special ultrasound stethoscope called a Doppler. The pressure in your foot is compared to the pressure in your arm to determine how well your blood is flowing and whether further tests are needed.
Because atherosclerosis is a systemic disease, individuals developing plaque in their legs are likely to have plaque building up in the carotid arteries, which can lead to stroke, or the coronary arteries, which can lead to heart attack. Early detection of PAD is important because these individuals are at significantly increased risk, and preventive measures can be taken.
An individual with an ABI of 0.3 (high risk) has a two- to three-fold increased risk of five-year cardiovascular death compared to a patient with an ABI of 0.95 (normal or low risk).
Ultrasound
Sound waves are used to measure blood flow in the arteries and determine whether there is a blockage.
Computed Tomography (CT) Angiography or Magnetic Resonance Angiography
Both tests produce images of arteries; the CT exam uses X-rays, while the MRA does not. For both exams, a patient may be injected with a dye or other contrast agent to make the arteries more visible.
Vascular Disease Testing And Screening
The Vascular Institute offers free ABI screenings. We invite you to schedule your ABI test today so that we can start your peripheral vascular disease treatment tomorrow.
If you do not currently have symptoms that does not mean you are not at risk for vascular disease. If you have risk factors such as:
- Age 65 or older
- Age 50 or older with high cholesterol, diabetes, or smoking history
- Strong family history of heart or vascular disease or aortic aneurysm
If you have symptoms you should consider getting an ABI test to see if they are related to peripheral vascular disease.
Symptoms include:
- Pain in the thigh, calf or buttocks with walking certain distances
- Non-healing wounds on your feet or lower extremities
- Pain in the leg or foot while resting relieved by hanging over the bed
PAD Patient Forms
If you have a PAD appointment, please print and complete the patient forms. Please bring the completed forms to your appointment.
Frequently Asked Questions About Peripheral Arterial Disease
Can peripheral arterial disease be prevented?
While there's no guaranteed way to prevent peripheral arterial disease, you can reduce your risk by:
- Quitting smoking
- Controlling blood pressure and cholesterol levels
- Managing diabetes
- Eating a healthy diet
- Exercising regularly
How often should I see my doctor for peripheral arterial disease follow-up?
The frequency of follow-up appointments will depend on the severity of your peripheral arterial disease. Your doctor may recommend regular check-ups to monitor your condition and adjust your treatment plan as needed.
Can stress affect peripheral arterial disease?
Stress can exacerbate peripheral arterial disease symptoms. Managing stress through techniques like meditation, yoga, or deep breathing can help.
What is the role of alternative therapies in peripheral arterial disease treatment?
While alternative therapies may offer some relief from peripheral arterial disease symptoms, it's important to consult with your doctor before trying any new treatments. Some alternative therapies that may be helpful include acupuncture and massage therapy.
What is the main cause of peripheral arterial disease?
The main cause is atherosclerosis, a buildup of fatty plaque in the arteries that narrows them and restricts blood flow.
How long does recovery from a minimally invasive peripheral arterial disease procedure take?
Recovery is generally quick. Most patients go home the same day and can resume normal activities within a few days to a week, though strenuous exercise should be avoided for a short period as advised by your doctor.
Can peripheral arterial disease recur after treatment?
Peripheral arterial disease can recur, especially if the underlying risk factors like smoking, high blood pressure, and diabetes are not managed. Adhering to lifestyle changes and medication is crucial for long-term success.
Why is early diagnosis of peripheral arterial disease so important?
Early diagnosis and treatment are critical to prevent the progression of the disease, which can lead to serious complications such as chronic pain, non-healing wounds, and in severe cases, amputation. It also significantly lowers the risk of heart attack and stroke.
-
“I especially owe a debt o f gratitude to Dr. Petruzzi and Dr. Adler for their skills and encouragement. ”
- Anonymous -
“I’m so grateful to have Dr. Petruzzi and his staff as part of the medical team treating and dealing with my newly diagnosis of PAD. He’s very sensitive, respectful, and most of all compassionate. Thanks for all you do ALWAYS! ”
- Anonymous -
“Dr. Jacinto Camarena is very knowledgeable, and he takes the time to fully answer all your questions and takes the time to explain everything. I highly recommend him. Also, the staff at AMI is great. ”
- Anonymous -
“It was a COVID-safe environment and the staff was very welcoming and professional. Dr. Watts has a vast knowledge of vascular issues and discusses the value of empirical evidence to support a sound strategy of treatment. His personality is positive, and his analysis is patient-specific. Highly recommend ”
- Anonymous -
“Dr. Schmidling was very patient and caring. He explained the process every step of the way and I never felt rushed or ignored. Great doctor and support staff! ”
- Anonymous -
“I saw Dr. Kim at the Brick Office. He was extremely knowledgeable, compassionate, and attentive to my medical issues. He was very patient explaining things to me using pictures and diagrams. Dr. Kim treated me like I was the most important patient he has! I am so happy to be his patient and I feel that I am in competent hands! Thank you, AMI for having ... ”
- Anonymous

